It is an honor to participate in your care. Your health, safety, and comfort are paramount to us.
Please do not hesitate to reach out if you have questions after reviewing these FAQs, What is Mohs Surgery?, and the Patient Forms.
Of course. We are a full-service Dermatology practice. We would be honored to assist you with evaluation and biopsy of suspicious lesions if not already done by your dermatologist or primary care physician. We are also happy to perform excisions and prescribe non-surgical treatments when Mohs surgery is not needed.
Shelby Coplen, PA-C, joined our experienced team in 2024. Shelby has practiced medical dermatology in Tucson since 2018. Taylor Foxworthy, PA-C, joined in 2025. They are experts in skin cancer screenings, non-surgical treatment of skin cancer, and treatment of rashes, psoriasis, rosacea, and acne.
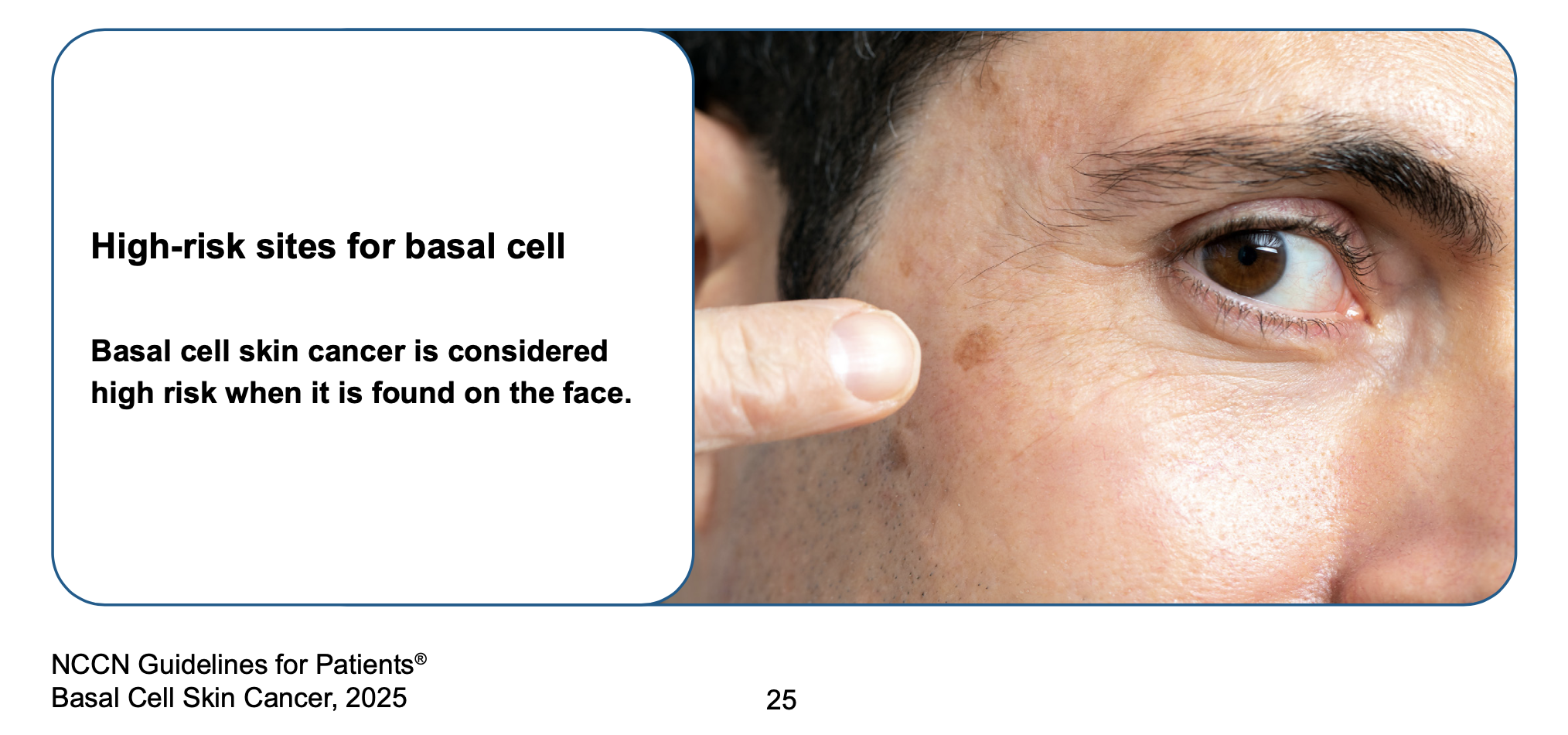
Mohs surgery is the gold standard and should be the initial therapy for skin cancers occurring in more cosmetically and functionally critical areas such as the face, ears, scalp, neck, hands, feet, and shins. Larger and more aggressive cancers in non-facial locations, as well as some “recurrent’ tumors (those that have failed other therapies) in lower-risk locations, are also appropriate candidates for Mohs surgery. Mohs surgery is also the best approach for skin cancers that are poorly defined, arise in a scar, grow rapidly, or occur in a patient with a compromised immune system in most locations. Mohs surgery is generally not needed for thin, small cancers in non-critical locations because these can be successfully managed with simpler techniques. Our team is happy to assist patients with cancers qualifying for Mohs surgery, simpler excision, or non-surgical therapies.
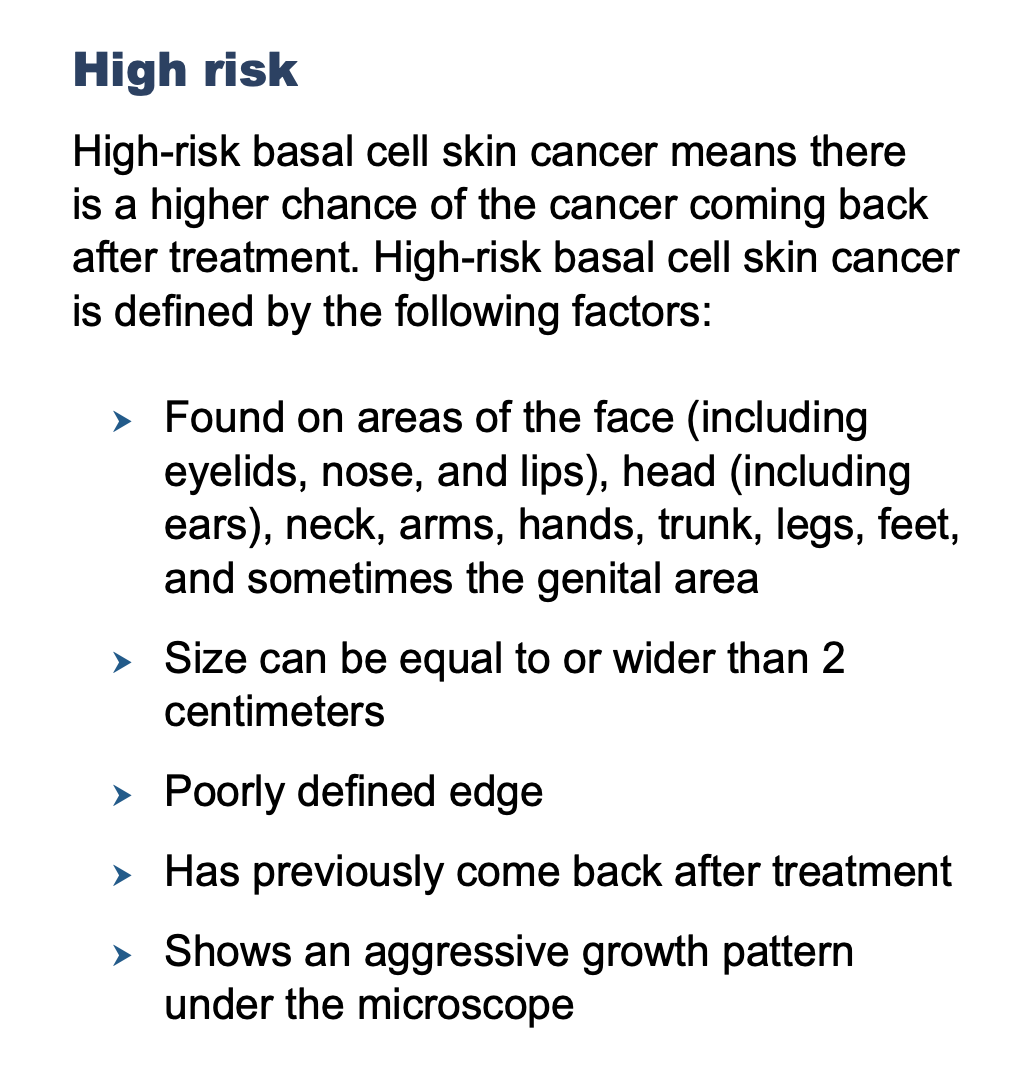
High-risk cancer as defined by the National Comprehensive Cancer Network (NCCN). Mohs surgery is the recommended INITIAL therapy for all high-risk tumors.
NCCN Patient Guidelines - Basal Cell Carcinoma
NCCN Patient Guidelines - Squamous Cell Carcinoma
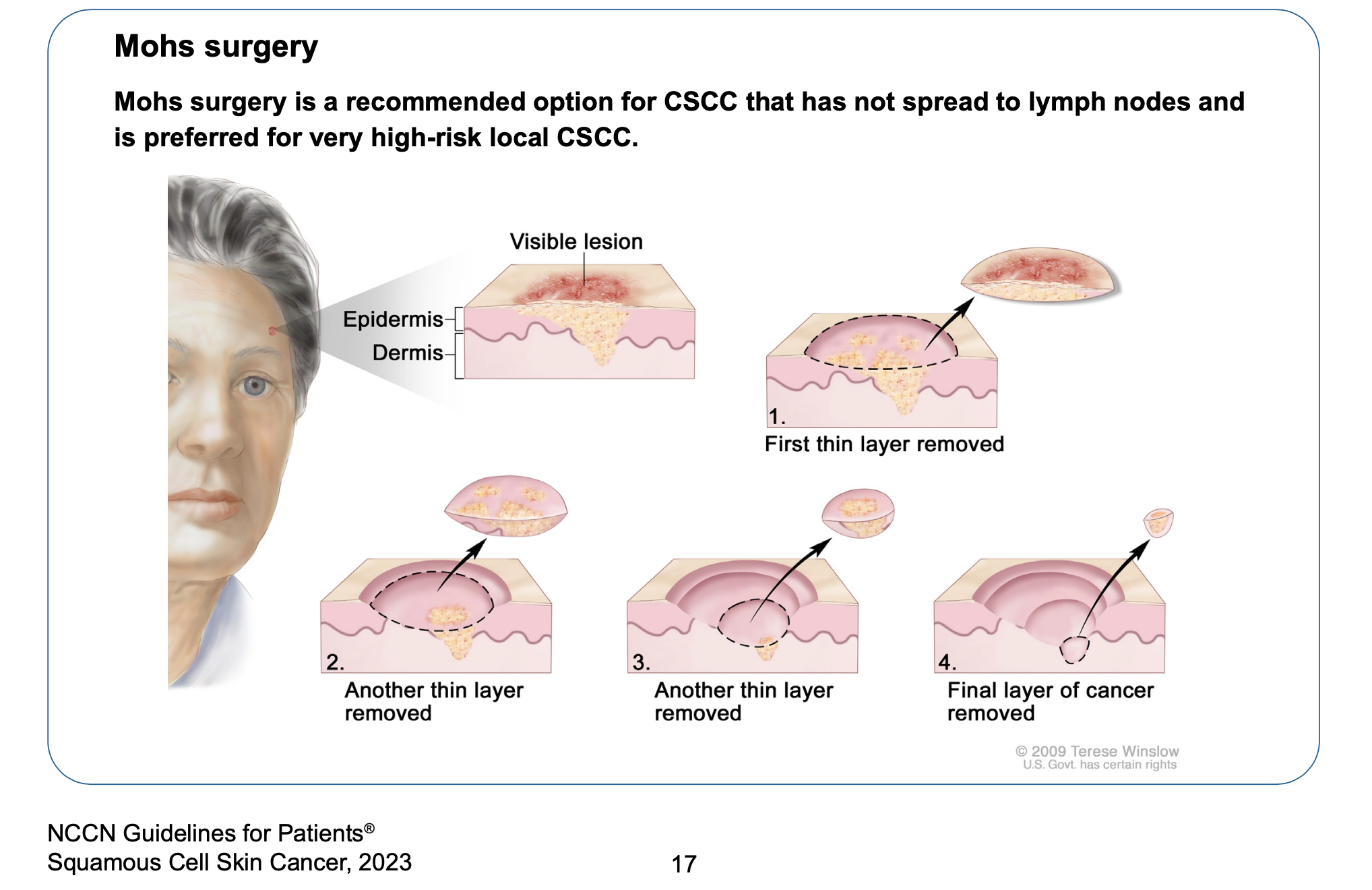
In Mohs surgery, one physician functions as both surgeon and pathologist. If a physician removes a skin cancer and sends the specimen to another lab or pathologist for analysis, he or she is NOT performing Mohs surgery for two reasons:
Yes. A biopsy removes only a small portion of the top of the skin cancer for diagnostic, not therapeutic, purposes. It does not remove the skin cancer roots, which are typically wider and deeper than what appears on the surface. This is the reason why microscopic analysis and precise mapping are the cornerstones of Mohs surgery. It's best to think of skin cancer like a weed where you have to remove all of the roots to kill the weed.
Mohs Surgery is a very accurate, office-based, outpatient procedure performed entirely under local anesthesia. It is best suited to small- to medium-sized skin cancers that have not yet invaded into important underlying tissues such as muscle, cartilage, nerves, or bone. Advanced tumors, those that have failed previous procedures, or those at higher risk of deep invasion or metastasis are often most safely and effectively treated by a hospital-based Surgical Oncologist. These advanced surgical cancer specialists have sophisticated training and expertise in larger surgeries and lymph node biopsies. They also have access to anesthesiologists and other specialists like Medical Oncology and Radiation Oncology who are often needed for more advanced skin cancers.
We have witnessed a worrisome trend in recent years in which high-risk tumors are initially and often repeatedly treated with less appropriate approaches such as "freezing", scraping ("ED&C"), "burning", radiation therapy, or creams when Mohs surgery should have been the initial treatment. These less accurate approaches are actively discouraged by organizations such as the American Academy of Dermatology, National Comprehensive Cancer Network, and American College of Mohs Surgery for the treatment of high-risk tumors such as those located on the face or in hair-bearing areas. Mohs surgery has been the gold standard for the treatment of high-risk tumors for decades.
Sadly, we are unable to accept referrals for many of these undertreated and mismanaged cancers. They often need drastic, large surgeries that are beyond the scope of our office-based practice. It is always best to diagnose and accurately treat ALL skin cancers as early as possible. Repeated failed therapies tend to turn small problems into much larger ones.
From the National Comprehensive Cancer Network. Mohs surgery is the recommended INITIAL treatment for all high-risk cancers.
Yes. Preoperative instructions may be found here.
Most patients spend 3 to 5 hours with us. Much of that is “downtime” where you rest comfortably while waiting on our team to prepare frozen Mohs sections and read the slides to ensure clear surgical margins. We encourage patients to bring reading materials to pass the time, and we also provide Wi-Fi access so that you may watch a movie or surf the internet on your own laptop computer, phone, or iPad. Please note that surgeries for larger, neglected, aggressive, recurrent, or mid-facial cancers may take longer, particularly if multiple stages are needed to clear the tumor and/or more advanced reconstruction is needed.
One of the biggest risk factors for sneakier tumor growth is a history of previous undertreatment, particularly freezing with liquid nitrogen cryotherapy. Unfortunately, freezing not only fails to cure the cancer but also tends to drive it deeper and wider into underlying tissues. Please note that these recurrent tumors typically require several Mohs stages to clear the tumor and need longer visits often lasting 5 to 7 hours.
The majority of wound closures are performed in our office. Occasionally, we may need to utilize an outside surgical specialist to perform the post-Mohs reconstruction if the tumor turns out to be larger, deeper, or more complex than initially anticipated. If an outside surgical specialist is needed, the reconstruction may take place on the same day or on subsequent days. Please note that it is safe to delay the reconstruction, and that it’s possible that hospitalization may be needed for extensive reconstructions.
Absolutely. Unlike some physicians performing Mohs surgery in Tucson, Dr. Dhir completed a dedicated and prestigious American College of Mohs Surgery (ACMS) accredited fellowship prior to entering private practice in 1999. He was then the single busiest Mohs surgeon in Kentucky for many years prior to opening Arizona Mohs Surgery and Dermatology in 2020. He has performed 46,000 Mohs procedures with a cure rate over 99.5% and an infection rate of only 0.2%. He carries subspecialty board-certification in Micrographic Dermatologic Surgery.
Dr. Dhir is a nationally recognized expert in both Mohs surgery and facial reconstruction. Since 2003, his colleagues have repeatedly elected him to both Best Doctors in America and Castle Connolly's Top Doctors - recognitions that place Dr. Dhir in the top 4 to 7% of all U.S. board-certified physicians, respectively.

We numb all of our patients prior to surgery to ensure your comfort. If you are a little anxious or we are doing surgery in the mid face, we also provide a small dose of an oral sedative to help you relax (“minimal sedation”). In that case, you will need to bring a friend or family member who can drive you home and remain with you for the remainder of the day. For larger cases, we also typically prescribe a few oral narcotic tablets to keep you comfortable for the first day or two after surgery when you may be sore.

You may have seen recent advertisements promoting superficial radiation therapy as an almost magical alternative to surgery for skin cancers. Some companies hide the significant radiation risks behind names like "Gentle Cure". Buyer beware. Most skin cancers are caused by too much radiation exposure. Therefore, it makes little sense to subject damaged skin to even more radiation for non-life-threatening tumors. Radiation therapy was first used over a century ago, and Mohs surgery was developed in the 1970's to provide a safer, more effective, and less costly alternative to the antiquated radiation therapy. Studies have demonstrated that cosmetic results are better for surgery than with radiation therapy for basal cell carcinomas less than 4 cm in diameter.
When radiation therapy fails to cure a cancer (the case in 8-20% of all treatments), surgery is no longer a great option because normal tissue has been damaged by the radiation therapy. This significantly limits a surgeon's ability to perform safe and effective reconstruction. Sadly, radiation therapy cannot generally be performed a second time because the risks of further tissue destruction are too great.
Mayo Clinic expressed significant concerns about superficial radiation (SRT) in the July 2025 issue of "Dermatologic Surgery": "Superficial radiation therapy is one of the oldest available treatment options for keratinocyte carcinoma, and its utilization declined with the increased effectiveness of surgical techniques. However, in the past decade, there has been a resurgence of dermatologists using SRT for treatment of keratinocyte carcinoma. Superficial radiation therapy is controversial as the American Society for Radiation Oncology's 2020 clinical practice guidelines recommend radiation therapy for patients who are unable to undergo surgical intervention. In addition, studies demonstrate a wide variation in 5-year local control rates, with SRT generally achieving lower control rates than Mohs micrographic surgery. Dermatologists should be aware of current guidelines that SRT is a second-line treatment option for nonsurgical candidates. In addition, dermatologists should consider equipping their practices with patient education materials that accurately and thoroughly present the pros and cons of both SRT and Mohs surgery to empower patients to make informed decisions regarding the treatment of their keratinocyte carcinoma. This approach will help prevent the spread of misinformation from publicly available sources on Google and other artificial intelligence chatbots."
We generally do NOT accept radiation recurrences for Mohs surgery in our office.

Nose, cheek, and chin severely damaged by radiation therapy for skin cancer

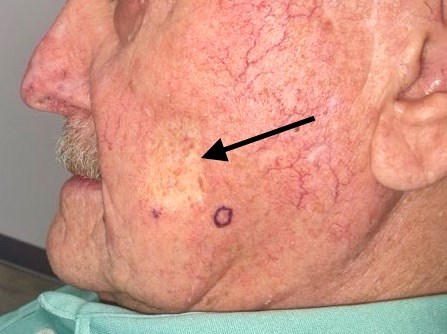
Recurrent left cheek basal cell carcinoma previously referred to us for Mohs surgery following failed radiation therapy. Note the permanent textural changes, abnormal pigmentation, scar tissue, and broken blood vessels caused by the radiation therapy. Surgical management is now very challenging because the radiation therapy has created a much more aggressive tumor AND destroyed background tissue needed for reconstruction.

White, depressed, mottled scar on left cheek caused by previous radiation therapy for skin cancer.
Similar, even larger, mottled scar on another left cheek caused by previous radiation therapy for skin cancer. This is permanent and will NOT improve with time.

Lasers can be successfully used to treat many structural skin conditions, such as broken blood vessels, vascular birthmarks, brown spots, unwanted hair, and even tattoos. Dr. Dhir has a degree in electrical engineering and previously taught a course on laser physics at Emory University. He used lasers to treat non-cancerous lesions for many years and also wrote laser questions for the American Board of Dermatology examination.
Unfortunately, there are no lasers currently shown to reliably treat skin cancer. The official American Academy of Dermatology clinical guidelines specifically state:
"There is insufficient evidence available to make a recommendation on the use of laser therapies or electronic surface brachytherapy in the treatment of basal cell carcinoma or squamous cell carcinoma."
https://www.jaad.org/article/S0190-9622(17)32529-X/pdf
https://www.jaad.org/article/S0190-9622(17)32530-6/pdf
Likewise, the National Comprehensive Cancer Network does NOT recommend lasers for the treatment of any skin cancer.
Patients are often biopsied by their dermatologist, primary care physician, or other surgical subspecialist and then referred to Dr. Dhir specifically for Mohs surgery. Shelby Coplen, PA-C, is also available to examine suspicious lesions and perform biopsies. Dr. Dhir and Shelby Coplen, PA-C, are specialists, and your insurance company may require that you secure a referral from your primary care physician before seeing a specialist. Therefore, please check with your insurance plan to determine if a referral is required. It’s also a good idea to check whether your insurance plan requires pre-certification or pre-approval for surgery with us.
It is actually safest for some patients to continue important blood thinners to minimize the risk of cardiovascular events. Fortunately, the risks of bleeding with Mohs surgery have been proven to be low even with blood thinners. In certain locations, we may ask patients to briefly discontinue blood thinners to ensure the best outcome. In the event that an outside surgical subspecialist will be performing the post-Mohs reconstruction, we ask that you please follow his or her recommendations regarding whether to stop your blood thinners.
In most cases, the wound is closed following successful excision of the cancer. This generally involves stitches on both the inside and outside of the wound. The stitches may dissolve on their own or require a return visit to our office in 7 to 21 days for removal. In some cases, the wound may be able to heal nicely without stitches. At the completion of surgery, we will provide you with detailed instructions on postoperative wound care depending on your reconstructive approach. A general sense of post-operative instructions can be found here.
Fortunately, basal cell carcinomas are generally slow growing and rarely "metastasize", or spread, to lymph nodes or internal organs. However, if ignored, they can grow to very large sizes and destroy surrounding tissue and organs. This occurs via compounding, in which each cancer cell divides every so often, making a copy of itself.
These are photos of neglected basal cell carcinomas. A cancer does not have to be deadly to warrant early and effective treatment.





Yes. Any surgical treatment, including Mohs surgery, creates a scar. A scar is the body’s natural way of healing after an injury. We will do our absolute best to minimize scarring. The length of the final scar is often greater than patients expect, because skin reconstructions are typically 2 to 3 times longer than the surgical defect size to eliminate puckering of the skin that occurs during closure. Your scar will soften and fade for several months after surgery, so please be patient as your body heals. You can greatly reduce the risk of suboptimal scarring by carefully following our pre- and post-operative instructions, especially with regards to avoidance of alcohol and tobacco consumption in the peri-operative period. Meticulous wound care and minimizing strenuous activities are also very important.
YES. After surgery, we ask that you return home and rest for the remainder of the day. Patients can usually shower after 1 to 2 days, but you should avoid swimming in a public pool, lake, or ocean for at least 2-3 weeks. Lighter activities and going for a walk are usually OK after 1 to 2 days, but it is important to limit strenuous physical activities, including golf, exercise, tennis, cycling, and yoga / Pilates, for 2 to 3 weeks to allow the wound to develop sufficient strength before being subjected to stretching and tension. This is very important to achieve the best possible cosmetic result which we believe is as important as curing your cancer.
The majority of Mohs surgeons and dermatopathologists believe that permanent (formalin-fixed) tissue sections allow more accurate margin analysis for melanoma than Mohs frozen sections, even if additional MART-1 immunostaining is done. This is not an issue for basal and squamous cell carcinomas, where frozen sections are universally accepted and allow more efficient, same day analysis. Therefore, we follow current NCCN surgical margin guidelines which state "the gold standard for histologic assessment of excised melanoma is use of permanent sections". Our specimens are evaluated within 24 - 48 hours by a board-certified dermatopathologist. NCCN guidelines also suggest that the surgeon consider delaying closure of melanoma excisions until margin analysis has been completed if a flap or graft may be required. This means that some melanoma surgeries may require 2 or more visits to ensure maximum accuracy.
Smaller squamous cell carcinomas are easily treatable and rarely pose a threat to life. Unfortunately, larger squamous cell carcinomas (greater than 2 cm in diameter) and those with more aggressive microscopic growth patterns can "metastasize", or spread, to lymph nodes and internal organs such as the lungs, liver, or brain. Patients are often surprised to learn that cutaneous squamous cell carcinomas typically cause twice as many deaths in the United States each year as melanoma (15,000 vs. 7,200). It is important to take all skin cancers seriously, including basal cell carcinoma, squamous cell carcinoma, and melanoma.
This is an unfortunate photo of a gentleman who presented to our clinic with neglected cutaneous squamous cell carcinoma that had already metastasized to surrounding skin, lymph nodes, and internal organs. His disease proved fatal.

Unfortunately, yes. After having one skin cancer, statistics show that you carry a higher chance of developing another skin cancer. In fact, if you have had 2 skin cancers, some studies suggest a 92% chance that you'll have a 3rd skin cancer. Therefore, it’s important to perform monthly self skin examinations and visit your referring physician for routine check-ups at least once each year. You can significantly reduce your future risk by practicing good sun protective measures and avoiding tanning beds and tobacco use. It’s never too late to develop healthier lifestyle practices because the human body has an amazing capacity for healing and regeneration.
Dr. Dhir and Arizona Mohs Surgery participate with Medicare and Medicaid (AHCCCS), as well as the majority of private insurance plans, including Aetna, AZ Complete Health, BCBS, Humana, United Healthcare, Ambetter, and Allwell. Health insurance plans and contracts continually change, so we highly recommend that you contact your insurance carrier to ensure that Arizona Mohs Surgery is a contracted provider with your specific plan. We are honored to serve our military men and women in uniform via our participation in Tricare.
We are currently credentialed with Cigna Medicare Advantage but NOT Cigna commercial. At present, the only other major plans with whom we are NOT contracted are Banner Network and Caremore.
On January 1, 2026, we will no longer be contracted with Humana.
If we are not participating providers in your commercial plan, you may still see us an out-of-network provider but this may cause you to incur higher costs depending on your insurance company’s policies. Please refer to our Financial Policy form for details regarding your financial obligations.
You may pay a bill via this website or in person. For your convenience, we accept cash, checks, Visa, MasterCard, American Express, Discover, and Visa Debit cards. We do not participate in Care Credit or offer any financing or payment plans.

Arizona Mohs Surgery is committed to providing the safest environment for both patients and staff. For decades, surgical facilities have been at the forefront of fastidious infection control practices due to challenges such as Hepatitis and HIV. To combat newer airborne diseases such as Covid-19 (SARS-CoV-2), we employ Global Plasma Solution’s NPBI air purification technology. This state-of-the-art system is utilized by prestigious medical institutions such as the Mayo Clinic, as well as Google, Harvard University, and the White House. Pathogen reduction testing results may be viewed here. Our eight procedure rooms eliminate the typical “recovery room” utilized by many Mohs practices, where patients are placed in a communal setting while waiting on slides to be processed by the lab.